The Agency’s Marina Fulcher discusses what digital health means for Australia.
This article originally appeared on Australian Association of Practice Management (AAPM). Marina has over 25 years’ experience in healthcare practice management and is a Clinical Reference Lead working with the Australian Digital Health Agency on the My Health Record.

Marina Fulcher, Clinical Reference Lead
Are well-connected systems that communicate with each other so that information flows seamlessly and is available to healthcare providers with a single keystroke a practice manager’s dream or can it be a reality? These systems hold the promise of no longer needing to fax or frantically call around to find out results for a patient who is in the consulting room.
In our 2018 daily lives, we are immersed in an ever-evolving digital world, and it is fair to say that digital health is here to stay. This series of articles over the next few editions of The Practice Manager will consider what digital health means for Australia, from a healthcare provider and a healthcare consumer (patient) perspective.
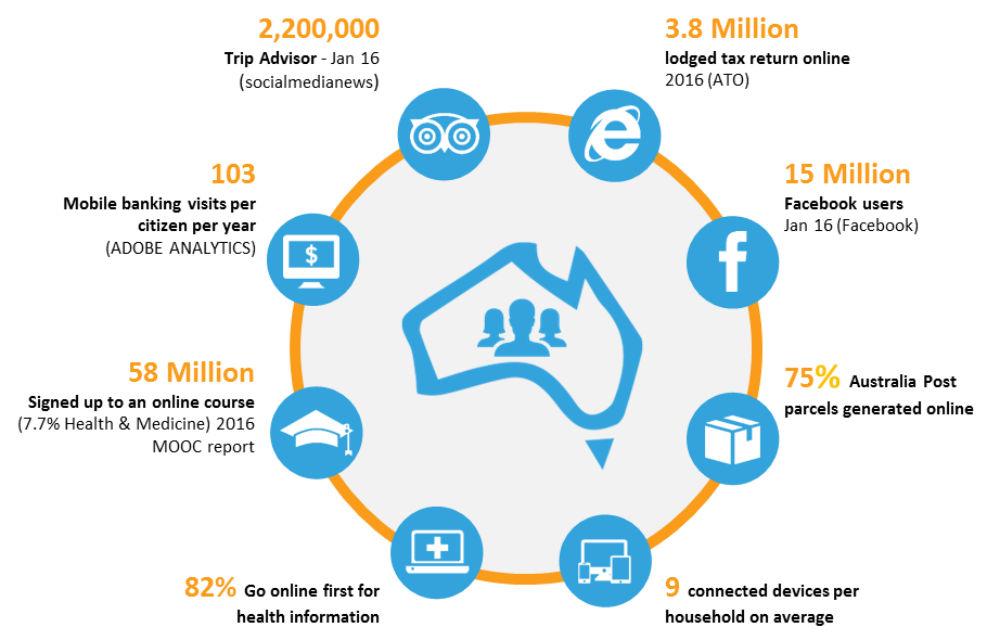
Australians are already digitally connected
So why is it that the benefits of a digitally enhanced healthcare environment is lagging so far behind other industries we interact with in our daily lives? There is no simple answer to this question. Perhaps it is due to fragmentation of healthcare in Australia. Perhaps it is because of the wide range of software being used by healthcare providers, or because of the highly sensitive information that is often involved.
Benefits of digital health
From the perspective of any patient but most particularly from that of someone with chronic and complex care needs, the benefits of not having to repeat their story or remember their medications every time they see a new healthcare provider are self-evident.
These benefits also extend to any healthcare provider, providing them with access to accurate and up-to-date information about the patient, who may be someone they have never met before and know nothing about.
Regardless of the type of practice you manage or work in – large or small, GP, allied health, specialist or hospital – it is critical for us to support safe and secure digital enablement in our practices and to ensure that the people working in our practices are aware of this and are appropriately trained.
The My Health Record system supports access to up-to-date information, with benefits as shown below.

My Health Record system benefits
Avoid adverse drug events: A recent key enhancement to the My Health Record is the Medicines View. A collection of medicines and allergy information from a number of places displayed on a single page.
Enhanced patient self-management: By encouraging patients to have a My Health Record and to refer to it, they will become more informed about their health and can be active partners in their care.
Improvements in patient outcomes: With access to up-to-date information, healthcare providers are assisted to make more informed decisions leading to improved patient outcomes.
Reduced time gathering information: Less time spent looking for information that has not been sent directly to the provider or has not yet arrived.
Avoid duplication of services: With the staged introduction of pathology and diagnostic imaging results to the My Health Record, the need for patients to have tests repeated will be reduced.
Foundations
As with any robust strategy, sound foundations need to be in place. Digital health is no different.
The Healthcare Identifiers Service that came into operation in July 2012 is a key enabler and one of the foundations for Australian digital health. It requires healthcare providers to be registered and have an individual Healthcare Provider Identifier (HPI-I) and the practice to register for an organisational Healthcare Provider Identifier (HPI-O). Whilst AHPRA registered professions are issued with a HPI-I, other professions will need to apply to the Department of Human Services.
Applications may be made through the Healthcare Identifiers Service for health professionals page on www.humanservices.com.au
Workflow
A major key to any change in work practises is to build the desired behaviour into the workflow. This will vary from one practice to another. Having well-connected systems will support ease of workflow and is a key to driving uptake of change, with the aim of reducing the burden of work, rather than increasing it. It is important to ensure that any systems that are used in practices are the latest available version to ensure that all users have access to any enhancements. Running out-of-date versions of clinical information systems, for example, will mean that, although they still access the Healthcare Identifiers Service and the My Health Record, the system has not been modified to provide access to any available new features.
The benefits of uploading Shared Health Summaries (SHS) is much more than meeting your practice’s 0.5% SWPE to qualify for the ePIP! By educating doctors to upload a Shared Health Summary (SHS) to a patient’s My Health Record as part of their usual consultation process, perhaps beginning with a focus on patients who have complex and chronic health care needs, is an excellent starting point.
“In our practice we use My Health Record widely. We are always trying to upload more, and as many patients’ information as we can. We have an active program to ensure practitioners are aware and conscious of that. Coming up in our in-house education series is a series on My Health Record and how to upload records, how to read records, and how and when to access records, so that all the doctors are aware and are able to use the My Health Record.”
- Townsville-based GP Dr Ron Malpas
Thereafter, an updated SHS would be uploaded for patients when there is a change to their diagnoses, medications, immunisations, allergies or adverse reactions. This SHS document is likely to be relied on by other healthcare providers your patients may see, particularly if they are travelling away from home.
Encouraging healthcare providers in your practice to review information in their patients’ My Health Record may also save time searching for information that may not have arrived at the practice, reducing the administrative burden that can often ensue as a result.
So what’s new?
Medicines View: The middle of 2017 saw the introduction of a key enhancement – the combined Medicines View. This brings together medicines information from many different sources including patient-entered information and discharge summaries displayed in a single view in the patient’s My Health Record. With this view it is possible to see what has been dispensed and what has been prescribed by other doctors, including changes to dosage and ceased medicines as well as allergies from all sources, including any entered by the patient or a discharge summary if the patient has been in hospital.
Pathology & Diagnostic Imaging results: Pathology and diagnostic imaging results are starting to be uploaded to My Health Record. Australia’s largest pathology laboratories and 95% of diagnostic imaging practices have agreed to start to connect to My Health Record and upload patient results. With patient’s having access to their results, they will be empowered to take increased control of their own health. From a practice perspective, results will continue to be received in the same way they are today and patients will have access to their results after seven days, allowing time for their doctor to contact them to discuss anything they need to with the patient.
More information
On demand training:
https://www.digitalhealth.gov.au/home/using-the-my-health-record-system/training-resources/on-demand-training
Read the blog from Dr Ron Malpas in full:
https://www.digitalhealth.gov.au/about-the-agency/digital-health-space/my-health-record-get-on-board